Solving scarcity through synergy: Inside one of Europe’s most integrated water technology ecosystems
Drinking water is a vital, but also finite resource in rapidly growing demand. And because of climate change, a growing population and the resource-intensive needs of both agriculture and industry, water scarcity is a growing problem around the world. In the TopDutch region, we have a unique watertech ecosystem of researchers and entrepreneurs working on world-class innovations and solutions to make sure we use the world’s most vital resource in the smartest and most efficient ways possible.

The city of Leeuwarden in the TopDutch province of Friesland is home to the WaterCampus, a global water tech hub with the internationally renowned research institute Wetsus and the Centre of Expertise Water Technology (CEW) at its core. It’s also home to the Water Alliance, a partner network that promotes and supports the business development activities of companies in the water and environmental technology sectors, from start-ups to multinationals, both nationally and internationally.
Unique in the world
“As a cluster and industry organization that’s part of the WaterCampus, the Water Alliance promotes and supports the business development activities of over 200 companies active in the water and environmental technology sectors”, says Ronald Wielinga, Executive Board Member and Manager Entrepreneurship at the Water Alliance. “We help companies of all shapes and sizes with things like national and international matchmaking, find funding opportunities, connections with technology partners and access to research facilities or national and international research and innovation programs”.

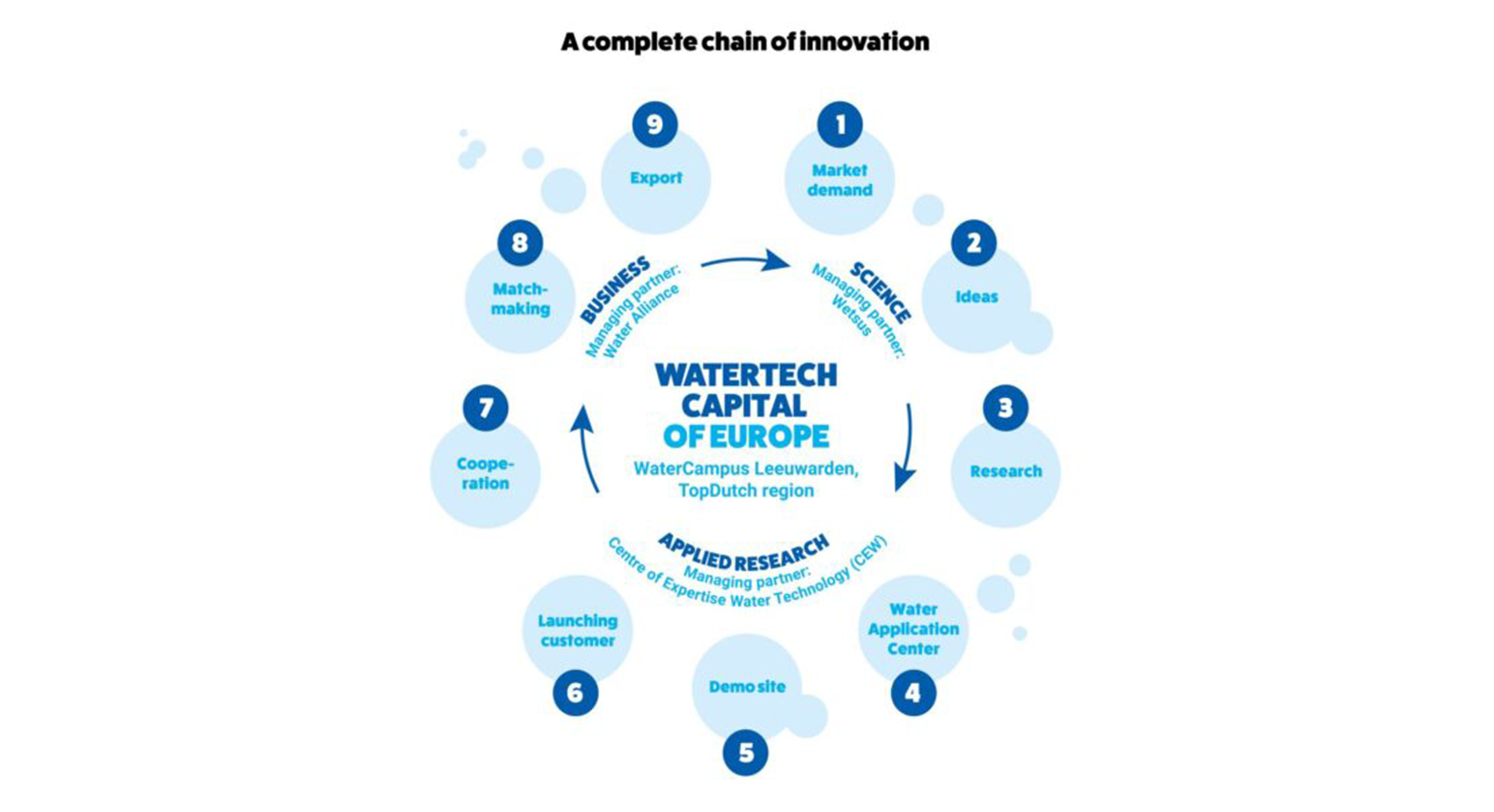
“What sets the WaterCampus apart as an ecosystem, is a unique synergy between research and entrepreneurship”, Wielinga continues. “It’s a multidisciplinary collaboration between companies and research institutes from all over Europe, along with all the necessary infrastructure and a fully developed innovation chain. We also work closely with other water tech hubs and leading research institutes around the world, to provide companies with international connections and access to new markets. In other words, we have everything we need here to make sure important circular water technologies can be developed, tested, upscaled and introduced in the global market. In terms of size and scale, I don’t think there’s a water tech hub like us anywhere in the world”.
What sets the WaterCampus apart as an ecosystem, is a unique synergy between research and entrepreneurship
Ronald Wielinga, Executive Board Member and Manager Entrepreneurship at the Water Alliance
From Wetsus research to the international market
“It’s a way of collaborating that helps set up important research for market success. Acquaint is a great example of a startup that came out of Wetsus research and is now active worldwide”, says Wielinga. “They develop ultrasonic technology to inspect water grids and are now active in the US, Asia, South America and Asia. And one of the founders also co-founded another Wetsus spin-off called HULO, that uses A.I. algorithms to monitor water distribution networks in real-time and prevent water waste”.
But it’s not just Wetsus spin-offs benefiting from the Leeuwarden water tech ecosystem. For Hydraloop, an internationally successful company that won the Best of the Best Award at CES Las Vegas in 2020 for their smart water recycling solutions for homes and businesses, the WaterCampus was a great launching pad. “They moved to the WaterCampus in 2017 for the testing facilities and the international network”, Wielinga says. “It helped them to further develop their technology, scale up production and have access to an international network. Hydraloop is a Dutch company of course, but we also see international water tech companies move to the WaterCampus for the same reasons, as well as for getting a good foothold in the European market”.
From Down Under to TopDutch
One of those international companies is Clean TeQ Water, one of the world's most innovative water treatment companies. They opened their European office in Leeuwarden and joined the Water Alliance in 2022. The ASX-listed Australian company has its headquarters in Melbourne and also has offices in China. “We provide innovative water treatment and metal recovery solutions for municipal wastewater, surface water, industrial wastewater and mining process water”, says Gerrit Boersma, Senior Process Engineer for Clean TeQ Water.
“We developed an ion exchange technology with automated resin transfer that was originally designed to help recover metals from water for the mining sector”, Boersma continues. “But the same principle can also be used for water treatment, making it a very efficient and cost-effective way to clean and re-use water. We specifically adapted the technology for high performance water treatment, to remove magnesium, sulphate, ammonia or nitrate from industrial wastewater for example, or to treat contaminated surface water. Outside of Australia, we were already active in China and the Middle East. The European market made sense as the next step for us, especially because of the new and stricter rules for wastewater treatment, phosphorus in particular, for which we have a great solution”.
It helped us get a good foothold in the European market and we plan to expand further. But it’s not just good for business, it's also about creating ways to solve urgent and real problems
Gerrit Boersma, Senior Process Engineer for Clean TeQ Water.
Chicken or egg
“But unlike, for example, in the Middle East, where it’s fairly common to do business remotely without the need to be physically located there, we realized the European market is different”, Boersma explains. “Our customers in Europe prefer local suppliers and having someone relatively close by in case they need support or if something doesn’t work as intended. And early on, that was somewhat of a chicken or egg dilemma for us. You need to have projects lined up to justify opening an office in Europe, but it also really helps to already have an office in order to get these projects. So which comes first? Fortunately for us, that sort of happened simultaneously, when we decided to open an office and landed contracts for two pilot projects in Belgium and Ireland”.

The choice to settle in Leeuwarden was a deliberate one, according to Boersma. “I was working in Melbourne, but I’m Dutch and so was our CEO at the time. So of course there was already some affinity with the Netherlands”, he says. “But we specifically chose Leeuwarden for its WaterTech ecosystem and the Water Alliance network, which allowed us to make interesting and meaningful connections with other water technology companies. And it was also great that we could make use of the lab facilities, to help set parameters for projects, but of course also to show our customers that our technology works. We have our own labs, but they’re located in Australia, so now we don’t need to ship our samples all the way over there first”.
“It helped us get a good foothold in the European market and we plan to expand further into Europe in the coming year”, Boersma continues. “But it’s not just good for business, it's also about creating ways to solve urgent and real problems, like water scarcity. And for us, that’s about more than just water treatment. We’re also very focused on creating value for whatever we extract from water, because you don’t want to end up with clean water and having a new waste stream. In the case of phosphorus for example, it’s a resource extracted through mining, which we use to make things like fertilizer, and it ends up in streams or surface water. We can extract it and dispose of it, but that also means losing a valuable resource you could use to make new fertilizer. We don’t want to solve one problem by creating another, so we’re very adamant about finding the best possible uses for everything we extract”.


